An Implantable Cardioverter Defibrillator, or ICD, connects to leads positioned inside the heart. These leads are used to deliver controlled electrical shocks to reset the heart should its rhythm become so abnormal as to be life threatening.
An Implantable Cardioverter Defibrillator, or ICD, connects to leads positioned inside the heart. These leads are used to deliver controlled electrical shocks to reset the heart should its rhythm become so abnormal as to be life threatening.
Implantable Cardioverter Defibrillator
Almost everyone’s heart skips beats or has moments where it beats faster or slower than normal. These mild palpitations are usually harmless, but more than 4 million Americans have recurrent episodes that need to be treated.
Some arrhythmia’s are treated with medicine, some with procedures like catheter ablations, and some with pacemakers. Still others are treated with Implantable Cardioverter Defibrillator, a device designed to quickly detect a life-threatening, rapid heartbeat coming from the bottom chamber of the heart. The device continuously monitors the heartbeats for regularity and delivers a shock to the heart when it senses a life-threatening rhythm.
An implantable cardioverter defibrillator has three main components:
- a pulse generator with batteries and a capacitor that can send a powerful shock to the heart;
- an electronic logic circuit to tell the implantable cardioverter defibrillator when to discharge; and
- fine wires, or leads, placed in the heart, to sense the cardiac rhythm and deliver the shock to the heart muscle.
Implantable Cardioverter Defibrillators also have a built-in pacemaker. Pacing may be necessary to support the heart in some instances, for example, after a shock, or during a very slow heart beat. The pacemaker also may allow the device to correct heartbeats that are too fast.
How does an implantable cardioverter defibrillator work?
Once the implantable cardioverter defibrillator is in place, the leads monitor your heart rate. If the device detects a dangerous heart rhythm, it sends out a controlled burst of impulses (called “overdrive” pacing). If that does not work, the implantable cardioverter defibrillator “shocks” the heart to restore a normal rhythm. Newer devices can also work like a pacemaker if a slow heart rate (bradycardia) occurs. When ventricular tachycardia or fibrillation occurs, the ICD records your heart rate, as well as the date and time of the event. It can also record what electrical therapy was needed to restore a normal heart rhythm.
What will I feel when my ICD gives me a “shock”?
A fast heart rate (see tachycardia) is usually corrected with very small electrical impulses. You may feel a flutter, palpitations (like your heart is skipping a beat), or nothing at all. Fibrillation (see ventricular fibrillation) may require that you receive a “shock.” Most patients say that the shock feels like a sudden jolt or thump to the chest. Some patients black out during fibrillation, so they may not feel anything when the shock is given. If someone is touching you while you are receiving a shock, they may feel a small muscle jerk, but it will not hurt them.
The heart
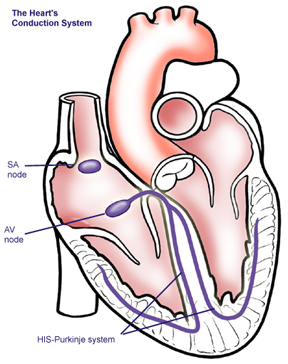 The heart is made up of four main cavities–the right and left atriums are the top two chambers of the heart and the right and left ventricles are the bottom chambers of the heart.
The heart is made up of four main cavities–the right and left atriums are the top two chambers of the heart and the right and left ventricles are the bottom chambers of the heart.
In a normal heart, the left and right sides of the heart beat together to maintain a steady supply of blood and oxygen to the rest of the body.
A typical heart beat begins with the sinoatrial node, a cluster of specialized cells located in your right atrium, firing an electrical impulse that spreads through the walls of the right and left chambers, causing them to contract, thus forcing blood into the lower chambers.
The impulse then travels to the atrioventricular node, another center of special cells located in the lower part of the right atrium. After a short pause, the pulses travels into the lower chambers, causing them to contract, forcing blood out of the heart to the lungs and body.
What can I expect as a Implantable Cardioverter Defibrillator recipient?
After you are diagnosed as a candidate for Implantable Cardioverter Defibrillator, you may be asked to stop taking certain medications several days before your procedure (such as blood thinners and aspirin). If you are a diabetic, you may be asked to adjust your diabetic medications. Do not eat or drink anything after midnight the night before the procedure. If you must take medications, drink only small sips of water to help you swallow your pills.
When you get to the hospital you will change into a hospital gown for the procedure, which will be performed in the Electrophysiology Lab. You will lie on a bed and the nurse will start an intravenous line to deliver medications and fluids.
You will receive a medication through your IV to make you very drowsy. The medication will put you to sleep. Due to the medications you will likely not recall the procedure afterwards.
This is completely normal.
Prior to the procedure, the nurse will connect you to several monitors that will allow the medical staff to monitor your condition at all times during the procedure.
The staff will clean and shave the area of the incision and you will be covered with a sterile cloth, after which the doctor will numb your skin by injecting a local anesthetic in the shoulder area. You may feel a slight pinching or burning feeling at first and then the area will become numb.
After you are numb, an incision will be made to insert the defibrillator and leads.
During the procedure, two very fine wires will be placed into a vein and the doctor will use a fluoroscopy machine (a special x-ray machine that allows the doctor to see your blood vessels), to guide them into the upper and lower right chambers of your heart. The lead tips are attached to your heart muscle. The other ends of the leads are attached to the pulse generator, which is placed under the skin in the upper chest, just below your shoulder.
After the leads are in place, the physician tests the leads to make sure lead placement is correct, the leads are sensing and pacing appropriately. This is called “pacing” and involves delivering small amounts of energy through the leads into the heart muscle. This causes the heart to contract.
After the leads are tested, the doctor will connect them to your Implantable Cardioverter Defibrillator. The pacing rate of your ICD and other settings will be determined by your doctor. The final settings are done after the implant using a special device called a “programmer,” which is used to put your heart into a fast rhythm so the doctor can watch as the device does its job–this all occurs as you are still sound asleep.
The procedure lasts about two to three hours.
After the Implantable Cardioverter Defibrillator implant?
After the implant, you will be admitted to the hospital overnight where your heart will be monitored for rate and rhythm. The following morning, you will sometimes have an x-ray to check your lungs and the position of your defibrillator.
Before being released from the hospital, your device will be tested one last time. The nurse or technician will place tiny electrodes onto your chest that attach to a computer monitor by a cable. A small machine known as a programmer is used to check your device. It has a wand that is placed directly over the device. This programmer allows the nurse or technician to read your device settings and make changes.
With these changes, the function of the device and leads can be evaluated. You may feel odd or feel your heart beating faster.
This is normal; however, report all symptoms to the nurse. Results of the device check are discussed with your doctor who will then determine your device settings.
Going home
Usually, you will be able to go home the day after your device is implanted. Your doctor will discuss the results of the procedure and answer any questions you may have.
Keep the area where the device was inserted clean and dry. The next day you may take a shower. Look at the area of the surgery daily to make sure it is healing. Your incision will be bound by surgical tape on the surface–leave these in place (the doctor will remove them at your follow up visit, though if they fall off on their own this is OK). Call your doctor if you notice unusual redness, swelling, drainage from your wound, or if you experience fever or chills.
You will be restricted in movement for the month following the procedure. You should not lift your elbow above your shoulder. You should not lift heavy objects. Activities such as golf, tennis and swimming should be avoided for six weeks after the device was implanted.
Despite what you may have heard, microwave ovens, electric blankets and heating pads may be used. Cellular phones can be used on the side opposite your device. You should receive a booklet with a lot of information about your device after surgery. If you do not, ask.
Directly after the procedure, you will receiver a temporary ID card that tells you what type of device and leads you have, the date of implant and the doctor who implanted it. In about three months, you will receive a permanent card from the company. It is important that you CARRY THIS CARD AT ALL TIMES in case you need medical attention at another hospital.
If you will be traveling through an airport, present this card to the security personnel and they will scan you with a portable wand, rather than require you to step through the walk-through detectors. (your device will set off the alarm). The wand will not damage the device.
Ask your doctor or nurse for more specific information regarding what types of equipment may interfere with your device.
Follow-up care
About two weeks after the procedure, you should see your doctor for a complete device check. This check is very important as adjustments will be made that can prolong the life of the device. You should also visit your doctor every three to six months following implantation to ensure everything is operating properly.
How often do I need to get my ICD checked?
After you get your ICD, you will have to go to the doctor for regular check-ups. ICDs can also be checked over the telephone. This is called transtelephonic monitoring. Even with telephone monitoring, you will still need to go to your doctor’s office for regular check-ups. The ICD is checked with a device called a programmer. When the programmer is held over the ICD, your doctor is able to tell if the ICD is working properly, how much power is left in the battery, and if the device has delivered therapy. The programmer can also be used to change the settings of the ICD. An ICD battery usually lasts between 4 and 8 years, depending on how many shocks it sends. When the battery runs down, a new ICD will be implanted. In most cases, your original ICD leads will not need to be replaced.
Will electronic devices affect my ICD?
If you have an ICD, you should always be aware of your surroundings. It is safe for you to be around wood working tools and normal home appliances, including microwave ovens. Stay away from heavy equipment that has very strong magnetic fields or strong electric fields (antennas, arc welders, and industrial equipment). Your doctor will help you understand what to avoid when you have an ICD.
Can I still drive a car if I have an ICD?
Many doctors will tell you not to drive for 6 months after your implantation surgery or after a shock. Talk to your doctor if you are not sure if it is safe for you to drive.
Can I use my cell phone if I have an ICD?
You should keep your cell phone at least 6 inches away from your ICD. When you are talking on your cell phone, hold it on the opposite side of the body from your ICD. Do not carry your cell phone in your breast pocket or on your belt if that means that it will be within 6 inches of your ICD.